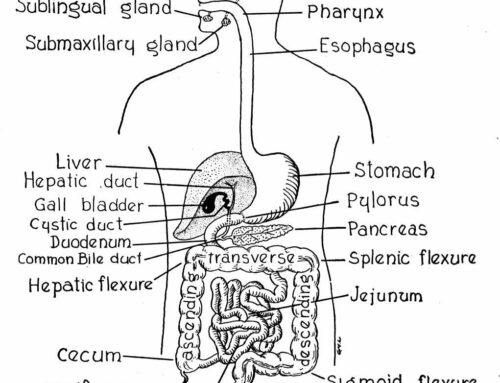
Our tour of the digestive system continues:
The action now moves into the small intestines. Since digestion is a north to south process whatever happened in the stomach will impact the small intestines. Did we digest our food or did it ferment? Are we taking antacids for acid reflux?
As the food or “chyme” as it is now technically called moves into the small intestines the stomach sends a signal to the pancreas informing it of the amount of carbohydrate, fat, and protein coming its way. The pancreas then prepares the required enzymes. Not to overstate the obvious, but the more work the stomach has done, the less the pancreas and the small intestines will have to do.
As you remember, the pH environment of the stomach is supposed to be acidic. However, the pancreatic enzymes only work in an alkaline environment. Secretions from the pancreas and bile from the gall bladder alkalinize the small intestine. The pH of small intestine should be 8.3. Without sufficient bile, the small intestines do not reach this pH.
Normally, food stays in the small intestine for 3-10 hours. During that time approximately seven liters of enzymes are produced – amylase, protease, and lipase. Ninety five percent of all digestion and absorption occurs in the small intestines. If the pH is not correct this will be compromised and transit time may be shorter (diarrhea) or longer (constipation). During this process 5.5 liters of the fluid is reabsorbed.
When working properly the digested molecules from the food we ate will be absorbed into the blood stream in the small intestines. Once in the blood it will fuel the body. The undigested material is passed on to the large intestine – our next stop.
What happens when food is not adequately digested and absorbed in the small intestines? There are two scenarios. First, food particles not digested well enough to pass across the gut wall pass down the alimentary canal, where they putrefy and form toxins that will be absorbed into the blood. Undigested carbohydrates feed the “bad” bacteria that we will meet later in the large intestines.
Or, the food particles are digested well enough to pass through the gut wall and into the blood, but are not reduced to particles small enough to be utilized by the body. This causes the intestinal mucosa to become inflamed which makes it more permeable. These are typically proteins. If you look at the major food sensitivities, intolerances, allergies, or whatever you want to call them, they are generally related to proteins: gluten from grains; casein from dairy, soy, and eggs.
What else contributes to an inflamed mucosal barrier? Studies show three major factors: therapy with prostaglandin inhibitors (NSAIDs, steroids, prednisone, and cortisone); antacids that decrease the acidity of the stomach, limiting the ability to digest proteins which leads to particles that get into blood leading to immune system reaction; and antibiotics that disrupt the normal balance of bacterial micro flora in the gut as well as the mouth, skin, and vagina leading to an overgrowth of bad bacteria and yeasts. NSAIDs are non steroidal anti-inflammatory drugs including ibuprofen, aspirin, and naproxen.
As poor digestion (dysbiosis) becomes your “normal” your intestinal permeability continues to increase and is then referred to as “leaky gut syndrome.” Healthy intestinal lining only allows properly digested foods to pass through into the bloodstream and be assimilated. It also keeps out bacteria and other foreign substances.
If the gut leaks these “things” get into the body a wide variety of symptoms and health problems are associated, including: abdominal pain, gas, indigestion, bloating, constipation, diarrhea, asthma, chronic joint pain, chronic muscle pain, confusion, fuzzy thinking, poor memory, mood swings, nervousness, aggressive behavior, anxiety, poor exercise tolerance, poor immunity, recurrent vaginal infections, skin rashes, bed wetting, recurrent bladder infections, fevers of unknown origin, shortness of breath, primary biliary cirrhosis, and general fatigue and malaise.
Bernard Rosen, PhD is a Nutrition Consultant and Educator. He works with individuals, groups, and at corporations to create individualized nutrition and wellness programs. He has offices in Coeur d’Alene, ID. To learn more or to schedule an appointment, e-mail at bernie@brwellness.com, call (208) 771-6570 or go to www.brwellness.com.